How can you observe if a wound is healing or not? In wound care, many indicators help a practitioner to see if a wound is improving or if changes to the wound care are necessary. Wound exudate (fluid) is one of these indicators. Exudate engages many of our senses and tells a descriptive story about the condition of the wound.
What is wound exudate and why is wound exudate important?
Wound exudate is fluid that leaks from the circulatory system via a wound and is usually triggered by inflammation. The body produces exudate in response to the release of local inflammatory factors (cytokines) caused by an injury. Inflammation causes the widening of blood vessels (vasodilation) and increased cell permeability for fluid to pass through, thereby producing more exudate [1].
Wound fluid is an essential part of wound management and is involved in all stages of wound healing [2]. The exudate can flush dead cells and microorganisms from a deep cavity and it helps in autologous debridement (natural debridement)*. Exudate carries components vital to the wound healing process. It for instance transports macrophages and neutrophils (white blood cells that can kill bacteria), and proteins to the wound. This is why wound experts agree that a wound bed should be kept moist to create an optimal wound healing environment.
Too much exudate indicates that there are underlying problems that will delay wound healing and may lead to biofilm formation and infection. It is essential to effectively assess the exudate and the type of wound to make an informed decision about a treatment plan.
Wound exudate, what does it consist of?
Exudate mostly contains white blood cells that protect the body against microorganisms entering the wound. It also contains many proteins and essential nutrients such as electrolytes and glucose, other inflammatory components, blood platelets, wound debris, metabolic waste products and microorganisms. The concentration of many of the beneficial components in wound exudate differs between healing and non-healing wounds.
Some components important for wound healing are explained below. Other relevant proteins are fibrin and fibrinogen (for blood clotting) and albumin and globulin (for osmotic pressure and transport of molecules).
Pro-inflammatory cytokines
Cytokines are proteins that are involved in the body’s immune response to an injury or infectious organism. They are secreted from immune cells and certain other cell types to stimulate inflammation. Some groups of pro-inflammatory cytokines are responsible for the passing of white blood cells from the blood vessels to the infected tissue to counteract infections.
Growth factors
Cells secrete growth factor proteins that support all kinds of chemical processes to heal tissue. Growth factors are chemical signallers to regulate growth, proliferation of cells and remodelling and strengthening of skin tissue. All stages of wound healing, especially the stimulation of cell growth, are regulated by these growth factors.
Matrix metalloproteinase (MMP)
To measure the progress in wound healing a certain type of enzyme is used: matrix metalloproteinase (MMP). The job of MMPs is to break down proteins when tissue is remodelled. In acute wounds, amounts of these protein-degrading enzymes are low and controlled. However, in a chronic wound with a long inflammatory period, the amount of these enzymes can increase. They degrade the proteins before they can effectively help healing. That is why high MMP-activity slows down wound healing.
Mitogens
Mitogens, or mitogenic activity, stimulate the division of cells (proliferation) such as fibroblasts (connective tissue cells), which are critical in all stages of wound healing, e.g. by stimulating the growth of new granulation tissue and skin tissue.
Non-beneficial components of wound exudate
Wound exudate also contains wound debris, metabolic waste products, and microorganisms [3]. These components do not have a function in the healing process. They may however delay wound healing if they are not transported to the surface of the wound where they can be removed.
Healing wounds versus non-healing wounds: what are the differences in wound exudate?
When we look at the concentrations of four of the exudate components (inflammatory cytokines, matrix metalloproteinases, growth factors, and mitogens) we observe differences in concentration levels between non-healing and healing wounds [4]. These differences give us good insight in why non-healing wounds don’t respond to standard of care treatment. Advanced wound treatments may be successful in restoring the balance. [4]
Table: Concentrations of exudate components in healing vs non-healing wounds
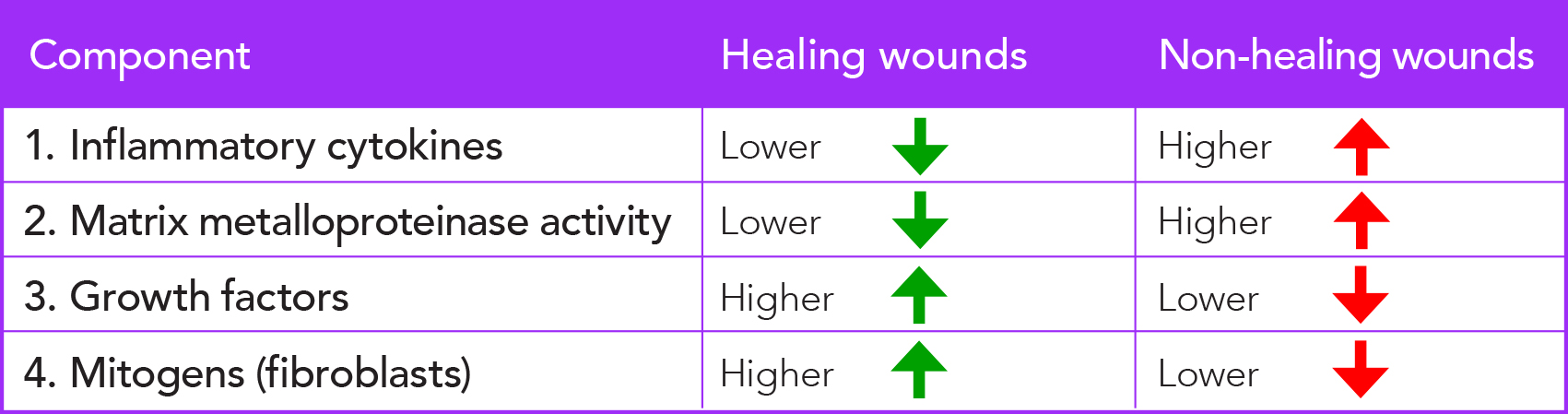
• A lower amount of inflammatory cytokines and MMP activity is beneficial to wound healing.
• A higher amount of growth factors and mitogens is beneficial to wound healing.
Biofilm and infection: what does wound exudate tell us about them?
The physical appearance of exudate, and the smell, can help determine if a wound is infected. For instance, a clear and thin exudate that changes to an opaque and discoloured exudate may be the result of an increase in bacterial growth in the wound. This indicates the wound might be infected. And a green, viscous exudate with pungent smell may indicate the presence of pseudomonas bacteria [4]. This observation helps to choose the correct treatment.
Clinicians should be aware of the fact that some dressing types change the characteristics of exudate. Some hydrocolloid and alginate dressings make the exudate look thick, because the dressing itself is becoming more gel-like.
The presence of biofilm can only be confirmed with microbiology testing, but at least 90% of chronic wounds have either a partially or fully formed biofilm [5]. Therefore, it is fair to assume that a biofilm will be present when treating a chronic wound, such as an ulcus cruris venosum or diabetic foot ulcer.
A mature biofilm** may cause an increase in exudate, but not necessarily. Biofilm delays wound healing by keeping the wound in a chronic inflammatory phase. This leads to increasing fluid accumulation in the skin tissue, which could increase wound exudate. A wound with biofilm will not necessarily be infected. The amount of exudate may be less in a wound with biofilm than in an infected wound.
How can you use wound exudate to your advantage?
Wound exudate may be used as an indicator of the wound’s status, a predictor if the wound will get better or worse. Additionally, evaluating the appearance, thickness, colour, smell, and amount of exudate helps the clinician to set up a treatment plan. In many clinics, it is not an option to continually perform wound cultures of open wounds. Based on the physical appearance of the exudate, it is possible to make a decision on which dressings / antimicrobials to use. Therefore, having the skills to critically assess wound exudate can positively influence the patient’s outcome.
There are great tools that can be used by practitioners to assess wound exudate. One very helpful guideline is the World Union of Wound Healing Societies (WUWHS) consensus document on the effective assessment and management of wound exudate [4].
Do you use wound exudate as a diagnostic tool when evaluating wounds? Is exudate and the appearance of a wound a good indicator for you for how to do wound care? Please post your reaction below.
* Read our blog on debridement
** Read our blog on biofilm
A notification on new blogs will be posted in our newsletter. Below you can subscribe.
References
[1] M. Spear, “Wound Exudate- The Good, the Bad, and the Ugly,” Plastic Surgical Nursing, vol. 32, no. 2, pp. 77-79, April/June 2012.
[2] P. Davies, “Exudate assessment and management,” Wound Care, pp. S18-S24, September 2012.
[3] K. F. Cutting, “Wound exudate: composition and functions,” British Journal of Community Nursing, vol. 8, no. 3, pp. 4-9, February 2003.
[4] World Union of Wound Healing Societies (WUWHS) Consensus Document. Wound exudate: effective assessment and management, Wounds International, 2019.
[5] A. a. Wolcott, “Clinically Addressing Biofilm in Chronic Wounds,” Advances in wound care, vol. 1, no. 3, pp. 127-132, 2012.


React