Written by Team Plasmacure
Antibiotics: Shooting a gun at a mosquito
Broad-spectrum antibiotics are often used routinely and long-term in the treatment of chronic wounds. This is shooting with a gun at a mosquito, while you would like to shoot sharply, so to speak. How can sharper shots be taken with antibiotics? The use of new DNA analysis techniques may help here. With this blog, we would like to offer our insight into this. We use a scientific article for this (ref. 1). This article describes how the bacterial community (wound flora) of non-closing wounds can be identified using a new DNA technique.
Using DNA techniques for antibiotic treatment: Why?
For targeted antibiotic treatment, you want to know which bacteria are present in an open wound. Cultivation methods allow the wound flora to grow over some time. However, because many bacteria are difficult to cultivate, these methods do not necessarily reveal the most common or most clinically relevant bacterial species.
Two separate studies (ref. 2,3) showed that culture methods failed to detect the dominant micro-organisms in more than 50% of the wound cultures analyzed. Furthermore, they detected only about 10% of the total micro-organisms present.
If you compare DNA techniques with culture techniques, it turns out that they are fast, comprehensive, sensitive, and specific. New DNA techniques show that bacterial communities are more complex than what culture methods show. Especially with chronic wounds the wound flora seems to be more complex. DNA techniques work by isolating DNA from bacteria present in wound fluid (exudate). Then a specific piece of DNA is multiplied until there is enough to measure. This is done using PCR techniques (polymerase chain reaction).
In many cases, there is no time to conduct a culture of an infected wound. To improve antibiotic therapy within wound care, the fast turnaround time of new DNA techniques can, therefore, be used.
A disadvantage is they cannot distinguish between living and dead cells (with culture methods they can). This can make the results difficult to interpret. Some comparable techniques mainly measure living cells, but these techniques have other drawbacks, which makes them less applicable.
Remarkable findings on wound flora in chronic wounds
In 2015 a study was published (ref. 1) that identified the wound flora (bacterial community) of 2,963 American patients with chronic wounds. This was done using DNA technique (16S rDNA pyrosequencing).
The chronic wounds were of the following 4 wound types:
1. 910 wounds on diabetic feet
2. 916 venous leg wounds caused by venous insufficiency (open leg, ulcus cruris venosum)
3. 767 bedsores (decubitus ulcer, pressure ulcer)
4. 370 non-healing surgical wounds
The study revealed the following findings:
• The number of bacteria types (diversity) and the ratio (“relative abundance”) of the different types of bacteria present in a wound are comparable between the wound types examined. Figure 1 shows which types of bacteria are present in which ratios on average in the different wound types. However, the amounts in which these bacteria are present can vary a lot between each wound (of the same wound type).
• Demographic data (gender, age, ethnicity, yes/no diabetic) do not affect the bacteria present in the wound types examined.
• Staphylococcus and Pseudomonas bacteria are most predominant in chronic wounds.
• Chronic wounds often contain bacteria that do not need oxygen (anaerobic) and commensals (bacteria that take advantage of the host without being adversely affected).
• Most wounds contain multiple bacterial species, only 7% contained only 1 bacterial species.
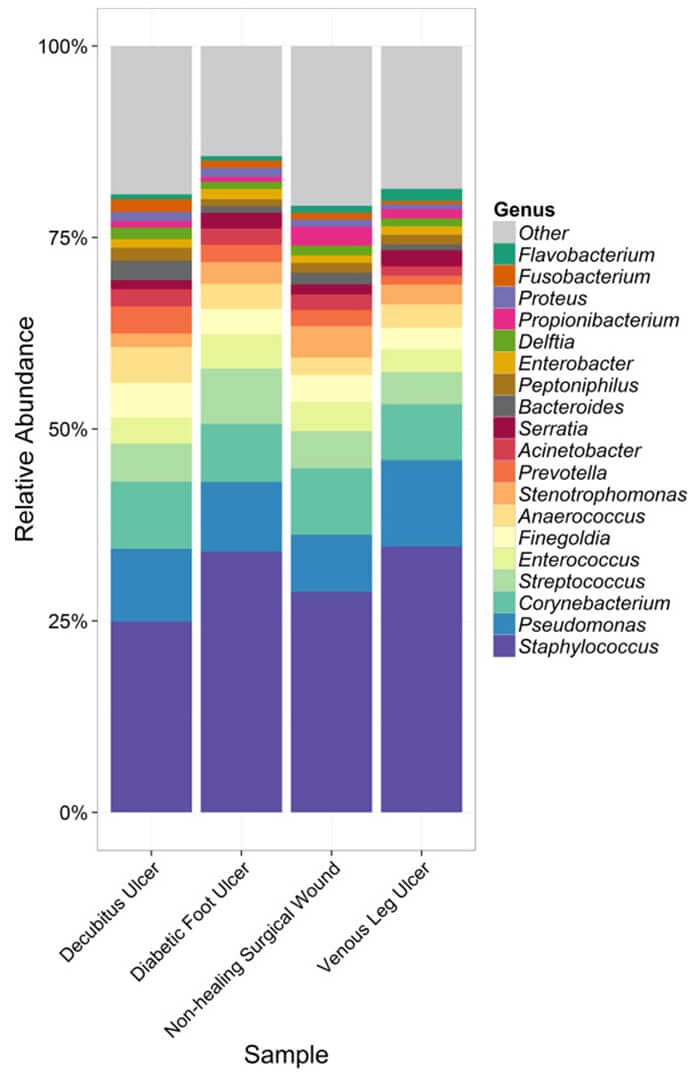
Figure 1: Proportions of the 20 most common bacterial species by wound type. Such as, the bacteria in pressure ulcers (Decubitus Ulcer) consist of an average of 25% staphylococci. Figure 1 is taken from Randall et al (2016) 1.
Are new DNA techniques clinically applicable?
The clinical applicability of these new techniques is not yet clear. DNA techniques can give a good insight into the presence of bacteria in a chronic wound (open wounds that do not heal). But we don’t know whether antibiotic treatment should target every isolated organism or just supposed bacterial “leaders.” Or maybe they should even target organisms that were once considered “lab weeds” and are likely to be non-pathogenic.
It is interesting to investigate whether existing DNA techniques can lead to more targeted antibiotic treatment of chronic wounds. Perhaps they can supplement or replace the well-known cultivation methods.
Do you consider it useful and feasible to use new techniques professionally to limit antibiotic use? We are curious if this information about wound flora is of interest to you for the treatment of chronic wounds. Please post your reaction below.
A notification on new blogs will be posted in our newsletter. Below you can subscribe.
References:
1 Randall et al; Analysis of the chronic wound microbiota of 2963 patients by 16S rDNA pyrosequencing; Wound Repair and Regeneration (2016) 24 163-174 © 2015 by the Wound Healing Society
2 Hoffman et al; Selection for Staphylococcus aureus small-colony variants due to growth in the presence of Pseudomonas aeruginosa; PNAS December 2006; 103(52):19890-19895
3 Fux et al; Survival strategies of infectious biofilms; Trends Microbiol. January 2005;13(1):34-40.
Other articles used:
• Emerson et al; Schrödinger’s microbes: Tools for distinguishing the living from the dead in microbial ecosystems; Microbiome August 2017; 5:86
• Lipsky et al; Diabetic Foot Ulcer Microbiome: One Small Step for Molecular Microbiology . . . One Giant Leap for Understanding Diabetic Foot Ulcers?; Diabetes March 2013; 62(3): 679-681.
• Nelson et al; Concordance in diabetic foot ulceration: a cross-sectional study of agreement between wound swabbing and tissue sampling in infected ulcers; Health technology assessment November 2016; 20(82):1-176
• Spichler et al; Microbiology of diabetic foot infections: from Louis Pasteur to ‘crime scene investigation’; BMC Medicine January 2015; 13:2
These articles have been interpreted by people from Plasmacure BV. Questions related to this blog are answered by our wound experts. Mail to blog@plasmacure.nl


React