Written by Team Plasmacure
Wound care protocols prescribe timely assessments to prevent long term wound care that is not being effective in healing of a wound (ulcer). Research shows that early initiation of advanced therapies improves healthcare outcomes; it can for instance accelerate wound healing and shorten hospitalization (Ref 1, Ref 2).
Knowing in advance that a given open wound is unlikely to heal despite standard care could enable care providers to make better decisions about treatment options (Ref 3) and could save the patient a lot of suffering.
How can you early identify which wounds heal with standard wound care and which need advanced therapies to heal? To identify this, there has been interest in finding markers that can predict wound healing at an early stage (prognostic tool). In this article we would like to give you more insight in some current tools to predict wound healing, coming from several scientific articles (see references).
Widely adopted prognostic tool to predict wound healing: Percentage wound surface area reduction
Patients in whom ulcer size fails to reduce by 50% over 4 weeks of treatment are unlikely to achieve wound healing over a reasonable period when using standard of care (Ref 4).
The often-quoted article from Sheehan et al. (Ref 4), describes that the 4-week healing rate predicts complete wound healing by 12 weeks. The wound surface area reduction over time (trajectory) for ulcers that eventually healed was clearly different from the trajectory for non-healers (Ref 2) as shown in Figure 1. By week 4, the percent wound surface area reduction (median) of the two trajectories were significantly different. In 91% of the cases, it was correctly predicted whether a wound would heal or not (sensitivity of 91%) (Ref 4).
Since then, 50% wound surface area reduction at 4 weeks has been widely adopted and confirmed as a robust indicator for predicting healing at 3 months, regardless of wound type (such as diabetic foot ulcer or venous leg ulcer (ulcus cruris venosum (Ref 5)).
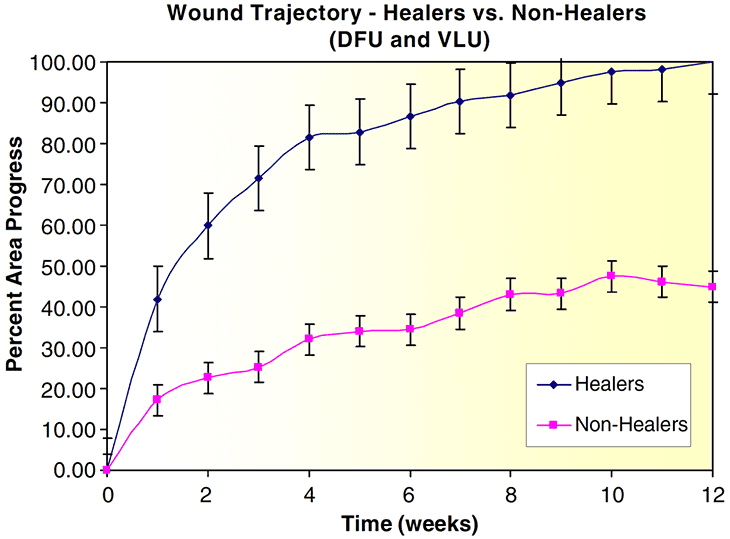
Figure 1: Wound trajectories for healers and non-healers in Diabetic Foot Ulcers (DFU) and Venous Leg Ulcers (VLU). The 100% percentage in the y-axis (Percent Area Progress) is the total wound closure. The progress in surface area reduction during 12 weeks is shown. De bars in the figure represent the standard error for each point. Figure 1 is taken from Ref. 6, 2008: Cardinal et al.
When using the 4-week 50% wound surface area reduction as an indicator, still about half of the diabetic foot ulcers with early healing progress do not heal by 12 weeks (Ref 7). Therefore, it is important to keep monitoring wounds also after the initial treatment period.
The monitoring of the wound surface area reduction after 4 weeks is in line with current wound care protocols (e.g. Ref 8.). These protocols advocate that all wounds should be initially (3-4 weeks) treated with standard wound care. When there is sufficient healing tendency, the wound still needs to be monitored until there is complete healing. When there is insufficient healing tendency, advanced wound care therapy is needed. These protocols are supported by Dutch insurance companies (Ref 9).
Development of new prognostic tools with big data
The tool described above is based on relatively small datasets obtained from clinical studies. Disadvantage of these clinical studies is that the settings in the clinical sites may differ from the real-world clinical settings (Ref 10). Nowadays computer controlled techniques (machine learning), applied to large clinical datasets (big data), can provide prognostic information about the wound healing tendency. These newer models do not need information over 4 weeks to predict wound healing, but they can rely on just one or two visits.
A published model that is based on the first two visits (Ref 11) showed a slightly better predictive accuracy than the model that is based on just the patient’s initial intake examination (Ref 3). In both studies wound level characteristics seem to be better predictors than patient level characteristics (demographics and comorbidities). The most important wound level characteristics include wound dimensions, wound tissue (granulation tissue, necrotic tissue) and the number of concurrent wounds. Palliative care also seems to be a very important parameter for the prognostic tool.
These more complex models are not intended to be applied directly by clinicians. Instead they are being developed as software tools (applications) within the Electronic Health Record system (medical patient dossier) and clinicians would use its output to help guide their management of wounds.
Conclusion: Predictive tools support accurate wound treatment
Research shows that early initiation of advanced therapies improves wound care outcomes, such as shorter time to wound healing and shorter length of stay. A prognostic tool may serve as a pivotal clinical decision point in wound management for early discrimination between patients who:
• may not respond to standard care (open wounds that do not heal) and may need advanced wound care therapy.
• respond well to standard care and do not need advanced wound care therapy.
This knowledge can be extremely valuable in costly and complicated wound management.
How do you determine if a wound is healing or not? After how much time of standard wound care do you evaluate whether the wound is healing sufficiently or may need advanced treatment? Please post your reaction below.
A notification on new blogs will be posted in our newsletter. Below you can subscribe.
References:
1 Baharestani et al. (2008); Early versus late initiation of negative pressure wound therapy: examining the impact home care length of stay. Ostomy Wound Manage. 54 (11):48-53.
2 Driver, V. et al. (2008); Health economic implications for wound care and limb preservation. J Managed Care Med. 1(11):13-19.
3 Jung et al. (2016); Rapid Identification of slow healing wounds. Wound Repair Regen, 24 (1):181-188
4 Sheehan, P., et al. (2003); Percent change in wound area of diabetic foot ulcers over a 4-week period is a robust predictor of complete healing in a 12-week prospective trial; Diabetes Care, 26(6): 1879-1882.
5 Frykberg, R.G. & Banks, J. (2015); Challenges in the treatment of chronic wounds; Adv Wound Care, 4(9): 560–582.
6 Cardinal, M., et al. (2008); Early healing rates and wound area measurements are reliable predictors of later complete wound closure; Wound Repair Regen, 16(1): 19-22.
7 Warriner, R. et al (2011); Differentiating diabetic foot ulcers that are unlikely to heal by 12 weeks following achieving 50% percent area reduction at 4 weeks; International Wound Journal, 8(6):632-637.
8 Kwaliteitsstandaard Organisatie van wondzorg in Nederland; verenig de expertise ten behoeve van de patient; 2018
9 Inkoopbeleid Regiefunctie complexe wondzorg 2021 en 2022, Zilveren Kruis.
10 Ennis, W. et al. (2017); Wound healing outcomes: Using big data and a modified intent-to-treat method as a metric for reporting healing rates; Wound repair Regen, 25(4):665-672.
11 Sang Kyu Cho et al. (2020); Development of a Model to Predict Healing of Chronic Wounds Within 12 Weeks; Adv Wound Care, 9(9): 516-524
These articles have been interpreted by people from Plasmacure BV. Questions related to this blog are answered by our wound experts. Mail to blog@plasmacure.nl


React